Making a Critical Illness Claim Process and Payouts: Your Essential Guide
Facing a critical illness diagnosis is a profoundly challenging experience, both physically and emotionally. Amidst the shock and uncertainty, the last thing you need is financial stress. That's precisely where critical illness insurance steps in, offering a vital financial safety net. But actually making a critical illness claim: process & payouts can feel like navigating a complex maze when you're at your most vulnerable.
This guide will demystify the entire journey, transforming the often-daunting claims process into a clear, actionable roadmap. We'll walk you through each step, from initial diagnosis to receiving your lump-sum payout, equipping you with the knowledge and confidence to secure the financial support you deserve.
At a Glance: Key Takeaways for Your Critical Illness Claim
- Prompt Notification is Key: Inform your insurer as soon as you receive a covered diagnosis.
- Documentation is Your Anchor: Gather comprehensive medical records, diagnosis reports, and personal ID. Organized paperwork is your best friend.
- Understand Your Policy: Know your specific covered conditions, definitions, waiting periods, and exclusions before you claim.
- Expect a Thorough Review: Insurers will meticulously verify your diagnosis against policy terms. This can take time.
- Payouts are for You: The lump sum is yours to use as needed – medical costs, recovery, living expenses, or income replacement.
- Don't Fear Denial: If denied, review the reasons, gather more evidence, and appeal. You have rights.
- Proactive Steps Pay Off: Being organized and communicative can significantly speed up the process.
Why Critical Illness Insurance Matters (And How It Works)
Critical illness insurance (CII) isn't about covering hospital bills like traditional health insurance. Instead, it's designed to provide a lump-sum financial payout upon diagnosis of a severe, predetermined medical condition. Think major events like heart attacks, strokes, specific cancers, or organ transplants.
The core purpose of this payout is to alleviate financial burdens, allowing you to focus squarely on recovery. This could mean covering direct medical costs not fully handled by your health plan, funding rehabilitation, adapting your home, or simply replacing lost income if you can't work. For many, it offers invaluable peace of mind during an incredibly stressful period. Understanding the payout process is crucial for ensuring efficient claim handling and timely financial support when you need it most. After all, what's the point of having a safety net if you don't know how to deploy it?
Your Step-by-Step Guide to Making a Critical Illness Claim
The journey from diagnosis to payout involves several critical stages, each requiring your attention. Let's break them down.
1. Diagnosis: The Starting Gun
The claims process officially begins the moment you receive a formal diagnosis of an illness covered by your policy. This isn't just a suspicion or a symptom; it's a confirmed medical finding from an authorized healthcare professional.
It’s crucial to remember that your policy will have very specific definitions for each covered condition. For example, a "heart attack" might be defined by certain enzyme levels and EKG changes, not just chest pain. A "cancer" might exclude early-stage or non-invasive forms. Familiarize yourself with these definitions early to manage expectations and understand if your diagnosis truly qualifies.
2. Filing Your Claim: The First Official Move
Once diagnosed, prompt notification to your insurer is paramount. Most policies have specified notification periods – sometimes as short as 30 or 60 days from diagnosis. Missing this window can complicate or even jeopardize your claim.
What to do:
- Contact Your Insurer: Call their claims department immediately.
- Request Claim Forms: They'll typically send you a claim package, which includes forms for you to complete and often forms for your treating physicians to fill out.
- Understand Deadlines: Note any submission deadlines provided by the insurer.
- Start Gathering Documents: This is where the real work begins.
Your Evidence Arsenal: Required Documentation
This step requires gathering comprehensive documentation. Accuracy, completeness, and organization are your guiding principles here.
Here’s what you’ll typically need:
- Proof of Diagnosis: The cornerstone of your claim. This includes:
- Detailed Medical Records: Hospital reports, doctor's notes, specialist consultations, lab results (e.g., blood tests, biopsies), imaging scans (X-rays, MRIs, CT scans), and pathology reports.
- Physician Statements: Forms completed by your treating doctors confirming the diagnosis, its severity, and the date it was established.
- Treatment Plans: Details of recommended or ongoing treatments.
- Proof of Identity: Government-issued ID (driver's license, passport).
- Policy Details: Your policy number and a copy of your critical illness insurance policy document, outlining your specific coverage.
- Financial Information: Bank account details for payout disbursement.
- Any Other Supporting Evidence: Depending on the illness, this might include rehabilitation plans, specialist reports, or proof of disability.
Best Practice: Create a dedicated folder (physical or digital) for all your claim-related documents. Make copies of everything you send to the insurer. Consider using a checklist to ensure nothing is missed.
3. Insurer Assessment & Verification: The Deep Dive
Once you submit your completed claim forms and documentation, the insurer begins its meticulous review process. Their primary goal is to confirm that your diagnosis aligns precisely with the policy's coverage and criteria. This isn't about questioning your illness; it's about ensuring contractual obligations are met.
What happens here:
- Initial Review: Claim adjusters will review all submitted paperwork for completeness and preliminary eligibility.
- Medical Professional Involvement: The insurer often appoints their own medical professionals or an independent medical reviewer. These experts play a vital role in validating your diagnosis, scrutinizing test results, and assessing the illness's severity against the policy's specific definitions.
- Corroboration: They may contact your treating physicians directly to verify information or request further clarification.
- Background Checks: In some cases, especially for larger claims, they might conduct background checks to ensure legitimacy and prevent fraudulent claims.
This stage requires patience. It's thorough by design, ensuring fairness and preventing misuse of the policy.
4. Medical Documentation Review: Aligning Your Story with Policy Terms
This step is a deeper dive into the medical specifics. Insurers systematically examine your medical records against the policy's exact definitions of covered illnesses. They’re looking for:
- Consistency: Do all reports tell the same story about the diagnosis and its progression?
- Authenticity: Are the documents genuine and from accredited healthcare providers?
- Completeness: Is there any missing information that prevents a full assessment?
They may request additional documentation or clarification directly from your healthcare providers, so maintaining clear communication with your doctors during this period is beneficial. They can help provide any supplementary information the insurer might need.
5. Claim Validity Determination: Does It Fit the Bill?
This is the decision point. Based on the extensive medical review, the insurer assesses whether your condition precisely aligns with the policy definitions. Key factors considered include:
- Timing: Did the illness occur after any waiting periods specified in the policy? Was it diagnosed after the policy was in force?
- Severity: Does the illness meet the severity criteria outlined (e.g., "loss of use" for certain conditions, or a specific stage for cancer)?
- Confirmation: Is the diagnosis confirmed by authorized medical practitioners using generally accepted medical standards?
If everything lines up, your claim moves forward.
6. Claim Approval: The Green Light
If all documentation is verified, and your condition meets all policy terms and conditions—including the onset date, severity, and confirmation by authorized medical practitioners—your claim is approved.
You will typically receive an official notification of approval, confirming that your claim has been validated and the payout is being processed. This is a moment of significant relief for many.
7. Payout Disbursement: Reaching Your Bank Account
Following approval, the payout is processed. This lump sum is usually disbursed via electronic bank transfers (EFT), direct deposits, or sometimes a check.
Crucial checks here:
- Verification of Payout Details: Ensure your bank account information provided is absolutely accurate to avoid delays.
- Disbursement Timelines: While approval can feel like the end, expect a few business days for the funds to actually reach your account. Policy terms govern these timelines, but typically it's within a reasonable period after approval.
This payout is generally tax-free in many jurisdictions, but it's always wise to consult a financial advisor for specific tax implications in your region. This financial injection can be a huge relief, allowing you to cover expenses and focus on healing without the added burden of economic worry. If you're wondering is critical illness insurance worth it?, receiving this payout often makes the answer a resounding yes for policyholders.
Why Critical Illness Claims Get Denied (And How to Prevent It)
A critical illness claim denial is disheartening, but understanding the common reasons can help you prevent it or prepare for an appeal.
Here are the primary culprits:
- Insufficient or Incorrect Medical Documentation: This is the most frequent reason. Missing reports, incomplete physician statements, or documentation that doesn't clearly confirm the diagnosis and its severity are red flags for insurers.
- Failure to Meet Specific Policy Criteria: Your diagnosis might be real, but it doesn't quite fit your policy's precise definition. For instance, an early-stage cancer might not meet the "invasive" criteria, or a minor stroke might not meet the required level of neurological deficit.
- Claims Filed Outside Designated Timeframes: Missing notification or submission deadlines specified in your policy can lead to denial.
- Suspicion of Fraud or Misrepresentation: Any inconsistencies, omissions, or misleading information provided during application or claim can lead to an investigation and outright denial. This includes pre-existing conditions not disclosed.
- Procedural Errors: Simple mistakes like incomplete claim forms, unsigned documents, or providing incorrect policy details can hold up or deny a claim.
- Waiting Periods/Exclusions: Your policy might have a waiting period (e.g., 90 days from policy inception) before certain conditions are covered, or specific exclusions (e.g., conditions related to self-inflicted injury). If your diagnosis falls within these, it will be denied.
What to Do If Your Claim is Denied: Your Right to Appeal
A denial isn't necessarily the final word. Policyholders have the right to appeal or refile. It's crucial to approach this process strategically.
Here's how:
- Review the Denial Letter Meticulously: This letter will state the specific reasons for denial. Understand every point. Was it a documentation issue? A definition mismatch? A timing problem?
- Gather Additional Supporting Documentation: Based on the denial reason, collect more evidence. This could mean:
- Updated Medical Reports: If the initial reports were unclear or incomplete.
- Clarifications from Healthcare Providers: Ask your doctor to write a detailed letter addressing the insurer's specific concerns, explaining how your condition does meet the policy definition.
- Expert Opinions: In complex cases, an independent medical review from another specialist might bolster your position.
- Submit a Formal Appeal: Draft a detailed appeal letter.
- Reference Policy Provisions: Clearly cite the specific sections of your policy that you believe support your claim.
- Attach New Evidence: Include all additional medical evidence.
- Explain Your Case Clearly: Articulate why you believe the initial denial was incorrect, linking your medical facts to the policy terms.
- Adhere to Procedures and Deadlines: Follow the insurer's specified appeal procedures and timelines meticulously. Missing deadlines here can be fatal to your appeal.
- Maintain Records and Communication: Keep copies of all correspondence—letters, emails, notes from phone calls (including date, time, and person spoken to). Document every step.
- Consider External Dispute Resolution or Legal Advice: If your appeal is unsuccessful, you may have recourse through external channels, such as an insurance ombudsman, a state insurance department, or by seeking legal counsel specializing in insurance disputes. This is usually a last resort, but it's an option.
Supercharging Your Payout Process: Best Practices for a Smooth Ride
While you can't control the diagnosis, you can control how efficiently you navigate the claims process. Adopting these best practices can significantly enhance your chances of a successful and timely payout.
Proactive Policy Review: Know Before You Need
The single most empowering step you can take is to fully understand your policy before you ever need to claim.
- Read the Fine Print: Familiarize yourself with all terms and conditions, eligible conditions, benefit amounts, stipulations, waiting periods, and exclusions.
- Understand Definitions: Pay close attention to how your policy defines each critical illness. These definitions are legally binding.
- Clarify Doubts: If anything is unclear, contact your insurer or a financial advisor to get answers. Knowing what you're covered for and under what circumstances avoids surprises.
Meticulous Record-Keeping: Your Documentation Diary
Think of your medical and claim records as a crucial narrative. An organized and complete story is easier to follow and verify.
- Centralized System: Maintain a dedicated folder (digital or physical) for all medical documentation. This includes diagnosis reports, test results, treatment histories, medical certificates, and physician statements.
- Accuracy is Paramount: Ensure all records accurately reflect your diagnosis, severity, and the necessity of treatment. Discrepancies can trigger delays.
- Track All Correspondence: Keep a log of every interaction with your insurer: dates, names of representatives, discussion points, and next steps.
- Digital Backups: Scan physical documents for digital backups, ensuring you have multiple copies.
Clear & Timely Communication: Keep the Lines Open
Effective communication with all parties is a force multiplier for your claim.
- Prompt Notification: Notify your insurer as soon as possible after diagnosis, adhering to their specified notification periods.
- Honest & Detailed Information: Provide clear, honest, and comprehensive information. Don't withhold details.
- Ask Questions: If you're unsure about a requirement, ask for clarification immediately.
- Collaborate with Doctors: Ensure your healthcare providers understand the importance of timely and thorough documentation for your insurance claim. They are key allies.
Adherence to Procedure: Dotting the I's and Crossing the T's
Following instructions to the letter might seem tedious, but it minimizes reasons for delay or denial.
- Follow Submission Requirements: Submit documents in the format and method requested by the insurer (e.g., online portal, mail, fax).
- Meet All Timelines: Be acutely aware of and adhere to all deadlines for submitting forms, additional information, or appeals.
- Complete Forms Fully: Never leave sections blank. If a question isn't applicable, write "N/A."
- Sign and Date Everything: Ensure all required signatures and dates are present.
After the Payout: What Comes Next?
Receiving your critical illness payout is a significant milestone, but it's not the end of your financial journey.
- Understand Financial Implications: While often tax-free, specific tax liabilities can vary by jurisdiction and how the funds are used. Consult a qualified financial advisor to understand any potential tax consequences or implications for other benefits.
- Strategic Use of Funds: The lump sum is flexible. Create a budget for how you'll use it to support your recovery, cover living expenses, adapt your home, or pay down debts.
- Review Your Policy: Depending on your policy terms, a critical illness payout might reduce your overall life insurance coverage or terminate the critical illness component. Understand the impact on your remaining insurance portfolio. You might need to assess your ongoing coverage needs for the future.
- Focus on Health Management: Use this period to prioritize your health, recovery, and well-being. The financial breathing room is designed to support this.
Frequently Asked Questions About Critical Illness Claims
How long does a critical illness claim typically take?
Claim processing time can vary significantly, ranging from a few weeks to several months. Factors influencing this include the insurer's internal procedures, the complexity of your medical case, the completeness and accuracy of your submitted documentation, and how quickly your doctors provide requested information. Staying organized and proactive in communication and documentation can help expedite the process.
Are critical illness payouts taxable?
In many jurisdictions, critical illness payouts are generally not considered taxable income because they are treated as a reimbursement for a personal loss (the illness). However, tax laws vary, and there might be exceptions or implications depending on your specific situation or how the funds are invested. Always consult a qualified financial advisor or tax professional for personalized advice regarding your region's tax regulations.
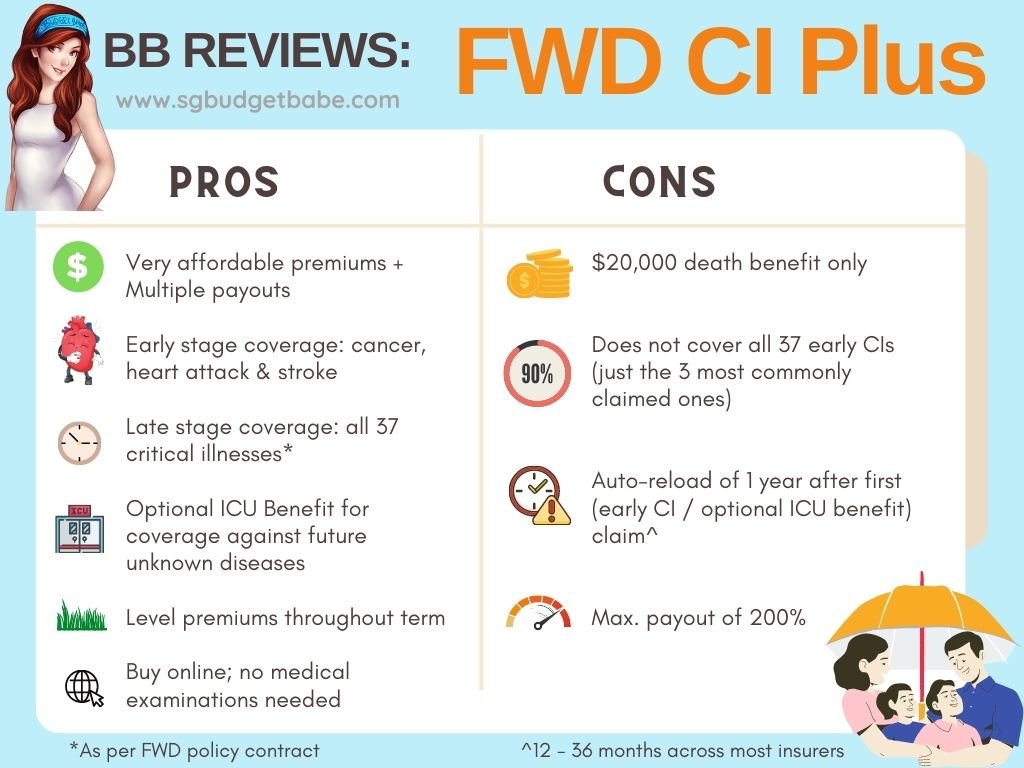
Can I make multiple critical illness claims?
This depends entirely on your specific policy. Some critical illness policies are "multi-claim" policies, meaning they may allow for claims for different, unrelated critical illnesses over the policy's lifetime, often with certain waiting periods between claims or aggregate limits. Other policies are "single-claim," meaning the policy terminates after the first approved critical illness payout. Always review your policy's terms and conditions regarding multiple claims.
Does a critical illness payout replace my income?
While a critical illness payout is not explicitly designed as an income replacement product (that's typically the role of disability insurance), it can effectively function as income replacement. Since the payout is a lump sum with no restrictions on its use, you can certainly allocate a portion of it to cover your lost income if you're unable to work due to your illness. This financial flexibility is one of its primary benefits, allowing you to prioritize recovery without immediate financial strain.
Your Roadmap to Financial Security During Illness
Navigating a critical illness is never easy, but securing your insurance payout shouldn't add to your burden. By understanding the process, meticulously preparing your documentation, communicating effectively, and knowing your rights, you can streamline your claim and focus on what truly matters: your health and recovery. Take these steps with confidence, and allow your critical illness policy to provide the financial stability it was designed for.